 How can we develop our workforce against a backdrop of cuts and challenges? DDN reports from the FDAP conference.
How can we develop our workforce against a backdrop of cuts and challenges? DDN reports from the FDAP conference.
‘Services are now expected to do more with less while caring for individuals with increasingly complex needs,’ said Carole Sharma, chief executive of the Federation of Drug and Alcohol Professionals, opening FDAP’s annual conference for workers in the sector.
So how could we drive workforce development to make sure that it was relevant and effective? First up was a well-known figure, Paul Hayes – formerly head of the National Treatment Agency (NTA) and now leading Collective Voice, representing treatment providers.
‘If we’re despondent about the state of the sector, odds are we’re going to be under-serving people,’ he said. ‘People say to me, can’t we have the NTA back – people who wanted to hang them from the nearest lamppost… but we have to get much smarter at tapping into a new narrative.’
Commissioners needed to be driving innovation and we had to make sure people had the skills to deliver. ‘We need to focus relentlessly on delivering outcomes,’ he said. ‘The most significant challenge for all of us is deaths – they’re going up very rapidly. We have to be ready to change our practice.’ Hayes acknowledged the climate of uncertainty, with no sign yet of when the drug strategy would come out. ‘Is all this easy and comfortable? No. But it is possible and necessary,’ he said, adding ‘If you think we’re all going to hell in a handcart, get out of this game.’
‘Nothing was ever positively done from despondency,’ said Pete Burkinshaw of Public Health England (PHE), who was keen to emphasise the sector’s ‘rich evidence base’. Another reason to be cheerful was localism, he said, as it ‘makes all of you much more important’. But with a growing cohort of people with complex needs, we had to develop specific competencies to manage the risks faced by service users.
‘Your doors need to be wide open to engage with need,’ he said. ‘Services can’t be a reflection of what we do, what we’re comfortable with and have always done. What you need is workers who have techniques and have belief in those techniques.’ As well as a set of universal core skills, workers needed meta competencies – and to ‘know when and where to do and not do things’ – an important element of adaptive and purposeful treatment.
FDAP had asked two of the larger treatment agencies how they prepared an effective workforce, so the conference heard from David Bamford from Change, Grow, Live (CGL, formerly CRI) and Guy Pink from Addaction. Pink believed it was ‘a really good time to be in the sector’ and described Addaction’s guiding principles as being ‘collaborative, ethical, inspiring, resilient and self challenging’ – ‘a team-based approach. We want people to be driven by integrity,’ he said, ‘so we recruit and manage against these guiding principles.’
The organisation was constantly reviewing challenges and solutions, looking at different patterns of working and ways of increasing productivity. ‘We’re doing more for less, but we have a good pool of workers,’ he said, emphasising that they did not want to be among the two thirds of the workforce who were disengaged. ‘We all know that people don’t leave organisations, they leave managers,’ he added, ‘so we’ve put a lot into improving managers.’
‘What’s difficult for staff to feel they manage is multiple requests from a lot of people wanting loads of different things,’ said Bamford. ‘We need to develop a growth mindset for our staff, as that’s what we want for people they work with.’ CGL believed that ‘top down doesn’t work’, he said. ‘We know that most people are interested in what’s going on around them or their first line manager. It’s pointless pitching things top down.’ So a flat hierarchy needed to go hand in hand with things that increased reliability – awareness of risk, expertise and the ability to adapt to the unexpected.
Staff were encouraged to reflect, plan, act, observe and evaluate, and were introduced to the ‘dreaded drama triangle’ during training – an illustration of how a worker can become a ‘rescuer, victim or persecutor’ in the workplace and recognise what triggers the situation. ‘Profound simplicity, such as five ways to wellbeing’ was also an aim, he said, ‘because simplicity of focus is effective.’
‘There was a positive side to being asked to do more with less, said Bamford, in that they were ‘also doing more with more – linking with people we’ve never linked with before.’ He also had a question for FDAP: ‘How do we extend the ladder downwards to the peer mentoring community, so people can work their way up?’
Sunny Dhadley, manager of Wolverhampton’s Service User Involvement Team (SUIT) was speaking next, and well placed to offer answers. He set up SUIT ten years ago, while still in active addiction and began attending meetings ‘where people were saying the same old rhetoric’. He realised that by sharing knowledge between his peer-led organisation and the workforce, they could develop competence and make treatment more compassionate. ‘We have a fantastic treatment system in this country and should be very proud of it – but we need to look at ways of doing more,’ he said.
‘Initiatives don’t need to cost the earth – we draw upon resources in society,’ he explained. With an annual budget ‘that costs less than sending an adult to our local cat B prison’, SUIT has worked with 522 different agencies and supported 146 people back into work in the past five years, as well as offering ‘a huge range of activities’. Top ten interventions have related to welfare, employment, education, emergency food, volunteering, housing, IT, healthcare, criminal justice and treatment.
‘We see a huge amount of inequality and low levels of literacy and numeracy,’ he said, mentioning that 24 per cent of prisoners had been in care as a child, with many having the English and maths skills of a primary child, so there were ‘high levels of vulnerability’. We needed to ask, ‘what are we doing to support people’s dream happening?’ he suggested.
Sam Thomas from Making Every Adult Matter (MEAM) added to the picture of working with people with multiple needs, talking about the ‘sheer complexity of the world that clients are trying to make sense of and that practitioners are trying to make work’. Around half of people with substance misuse issues also had another problem such as offending or homelessness, but we were ending up with services that dealt with one problem at a time.
‘We have a system that deals with numbers, but behind every number is a human being,’ he said. The MEAM project, Voices from the frontline, was trying to build a better dialogue between people making decisions and those affected.‘This often requires people to work in a way they may not have thought about or feel comfortable with,’ he said.
‘The family workforce could be an important part of this, said Oliver Standing from Adfam, who challenged the perception of families being ‘a bit of an add-on’.
‘The family workforce can be hard to pin down – they could be a service, a standalone community group, a carers’ centre, volunteers, drug and alcohol workers or a generic service – there’s no standard qualification but lots of dedicated people in it,’ he said. Whatever their background, they needed to be competent, trained, supported and connected to local services, including police, bereavement and mental health services.
‘Like others, we’re being asked to do more for less,’ he said, and ‘very high regional variation’ meant there was even greater need for drug and alcohol services to be trained to work with families. Adfam worked with decision-makers, practitioners and families and helped the three strands of activity to feed into each other. ‘There’s no gigantic evidence base on family support,’ he said. ‘But there’s something so affirming when families can meet someone in a similar situation who may be able to help.’
At the heart of effective outcomes were commissioners, and Fiona Hackland, strategic commissioner from the London Borough of Newham, shared her thoughts. ‘Commissioning is not just buying services, it’s a much more complex task,’ she said. ‘It’s about identifying what’s needed locally across services and making sure provision is in place to meet those needs.’ There was no qualification for commissioners, other than relevant components of DANOS. Local authority people were not used to commissioning health-based responsibilities and didn’t necessarily understand the process. ‘We can get bogged down in numbers and targets, but we need to focus on the differences we want to see,’ she said.
Funding was ‘clearly an issue’, with having to find savings from the public health grant, and the changing profile of substance misuse was an ongoing challenge. Reprocurement cycles were going to get worse, with short contracts causing ‘huge problems among service users’. Not viewing the commissioner-provider relationship as a partnership was also ‘not helpful’.
So how could commissioners ensure effectiveness?
‘Be clear about needs, prioritise needs and find the best way to meet those needs,’ she said. Specifying the service and outcomes we wanted was important – ‘without over-specifying, as that kills innovation’ – as well as taking service users’ views into account. For those worried about the added pressures of CQC inspection since April, Patti Boden, CQC inspection manager, had words of encouragement.
‘I don’t go out looking for inadequate services – we go out looking for good,’ she said. ‘How open are they with commissioners? We’re trying to make sure services are well led, with clear vision and values and performance targets, KPIs and visible leadership. ‘We’re also looking to see that the recovery agenda is at the top of their list,’ she said, adding ‘this is not a tick list, but around evidence from service users.’ Among the elements for improvement were risk, care/recovery plans that were too generic, and the quality of commissioning and clinical interventions. ‘We tell you where you’re going wrong, but we don’t tell you how to fix it – that’s up to you,’ she said.
Taking stock of the day’s contributions, Carole Sharma asked ‘do we need to rethink the skills and knowledge of the effective practitioner?’
‘We’re facing an aging client population, multiple and complex needs, reduced generic services and a simplified view of what alcohol and drug problems are and how to fix them,’ she said.
It was more complicated than ‘just say no’ and a spell in rehab, with ‘entrenched problems’. Reduced budgets for training and development, reduced learning environments for some licensed practitioners such as doctors, large caseloads and the demands of the regulator were constant challenges – although the demands of the regulator were a step in the right direction ‘as they stop a lot of arguments about what is good’. But there were a lack of national drivers for workforce development and still no national qualification framework.
‘What are the questions we need to consider?’ she asked. ‘What’s the best use of trained specialists’ time and competence? Do we broaden our skills and knowledge to meet the emerging needs of clients and patients? Do we use our specialists to support the generic health and care workforce in relation to alcohol and other drugs? Has DANOS had its day?’
Appealing to the audience – and the profession as a whole – she added, ‘Is there a need for FDAP to change? If you do feel you need a professional organisation, a safe space to develop the workforce, you need to get people to join.’
New paradigms
We need to go beyond training to tackle workforce development, says Professor Ann Roche
The workforce is without doubt the most important element in addressing alcohol and other drug (AOD) related problems.
Without an appropriately skilled, competent and confident workforce able to execute evidence-based interventions and policies the AOD sector will always be hampered in its efforts to prevent and ameliorate the ever changing array of issues. Ensuring that our services, programmes and policies offer best available options requires our workforce to be able to function to maximum effectiveness in increasingly challenging environments.
 Traditional thinking has relied heavily on training as a mechanism by which to achieve optimal service delivery, but while training is a necessary component in this complex picture, it is insufficient in itself. Research increasingly indicates major flaws in the ‘train and hope’ approach to knowledge transfer and innovation dissemination. That is, training often fails to deliver the ultimate expectation and goal – ie behaviour change. This is through no fault of the individual worker, as a multitude of factors are at play when attempting to change workers’ behaviours.
Traditional thinking has relied heavily on training as a mechanism by which to achieve optimal service delivery, but while training is a necessary component in this complex picture, it is insufficient in itself. Research increasingly indicates major flaws in the ‘train and hope’ approach to knowledge transfer and innovation dissemination. That is, training often fails to deliver the ultimate expectation and goal – ie behaviour change. This is through no fault of the individual worker, as a multitude of factors are at play when attempting to change workers’ behaviours.
In recent times an important paradigm shift has occurred, as training has been reconceptualised with the broader, more diverse and more comprehensive concept of ‘workforce development’. This is a multi-faceted approach, which addresses the range of factors impacting on the ability of the workforce to function with maximum effectiveness in responding to alcohol and other drug-related problems. Workforce development should have a systems focus; unlike traditional approaches, this is broad and comprehensive, targeting individual, organisational, and structural factors, rather than just addressing education and training of individual mainstream workers.
Without tackling the broad array of systems factors that determine and shape what workers and services can do we will be forever limited to ineffective, costly and inappropriate responses. A workforce development approach that incorporates a systems perspective allows issues related to social equity and work conditions, government policies and organisational structures to be seen as central. It then allows other factors such as worker wellbeing, recruitment and retention, career pathways, supervision and support to be addressed as pivotal concerns in regard to knowledge and skill transfer.Without taking this broader approach, transient training programmes will continue to soak up limited funds and produce relatively modest, if any, change in services and programs.
Although it may seem counter-intuitive that training alone cannot deliver pressingly needed changes and supports to our crucial AOD services, the evidence is abundantly clear. Training is, and will always be, only a small part of the solution. A broad and comprehensive workforce development approach that focuses on systems issues is what is required.
For further details and resources visit NCETA’s website: www.nceta.flinders.edu.au
Professor Ann M Roche is director, National Centre for Education and Training on Addiction (NCETA), Flinders University, South Australia
 Kevin Stow, an ex-drug user and previous hepatitis C sufferer shares his experiences and talks about how being cleared of hepatitis C helped give him the momentum to overcome his drug addiction.
Kevin Stow, an ex-drug user and previous hepatitis C sufferer shares his experiences and talks about how being cleared of hepatitis C helped give him the momentum to overcome his drug addiction.













 transmission. Meanwhile, the Glasgow City Alcohol and Drug Partnership (ADP) has established a working group to look at opening a facility in that city, along with plans for heroin-assisted treatment.
transmission. Meanwhile, the Glasgow City Alcohol and Drug Partnership (ADP) has established a working group to look at opening a facility in that city, along with plans for heroin-assisted treatment. Children watching England and Wales matches during the group stages of Euro 2016 were exposed to alcohol advertising every 72 seconds, according to research by Alcohol Concern. Pitch-side adverts for tournament sponsor Carlsberg appeared an average of 78 times per game, says the charity, with around 14 per cent of the audience likely to be under 18. ‘Alcohol marketing drives consumption, particularly in under-18s, and sport should be something which inspires active participation and good health, not more drinking,’ said the charity’s campaign manager, Tom Smith.
Children watching England and Wales matches during the group stages of Euro 2016 were exposed to alcohol advertising every 72 seconds, according to research by Alcohol Concern. Pitch-side adverts for tournament sponsor Carlsberg appeared an average of 78 times per game, says the charity, with around 14 per cent of the audience likely to be under 18. ‘Alcohol marketing drives consumption, particularly in under-18s, and sport should be something which inspires active participation and good health, not more drinking,’ said the charity’s campaign manager, Tom Smith.



 Traditional thinking has relied heavily on training as a mechanism by which to achieve optimal service delivery, but while training is a necessary component in this complex picture, it is insufficient in itself. Research increasingly indicates major flaws in the ‘train and hope’ approach to knowledge transfer and innovation dissemination. That is, training often fails to deliver the ultimate expectation and goal – ie behaviour change. This is through no fault of the individual worker, as a multitude of factors are at play when attempting to change workers’ behaviours.
Traditional thinking has relied heavily on training as a mechanism by which to achieve optimal service delivery, but while training is a necessary component in this complex picture, it is insufficient in itself. Research increasingly indicates major flaws in the ‘train and hope’ approach to knowledge transfer and innovation dissemination. That is, training often fails to deliver the ultimate expectation and goal – ie behaviour change. This is through no fault of the individual worker, as a multitude of factors are at play when attempting to change workers’ behaviours.
 A partnership between Blenheim and Club Soda aims to change drinking habits
A partnership between Blenheim and Club Soda aims to change drinking habits






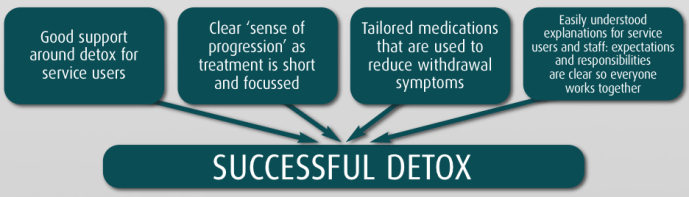






 providing a safe, supported environment, which is inclusive, structured and fair. We offer an holistic programme which addresses the physical, mental, emotional and spiritual wellbeing of each individual. We have a professional, qualified and trained team, with good boundaries and good ethical practice.
providing a safe, supported environment, which is inclusive, structured and fair. We offer an holistic programme which addresses the physical, mental, emotional and spiritual wellbeing of each individual. We have a professional, qualified and trained team, with good boundaries and good ethical practice. This is achieved via voluntary work placements or training courses and allows clients to demonstrate greater responsibility and independence.
This is achieved via voluntary work placements or training courses and allows clients to demonstrate greater responsibility and independence.








 expensive testing of the substances in specialised laboratories, and there is simply no budget big enough to carry out the work. A legal logjam awaits. Yet these drugs are not safe: users of synthetic cannabis are 30 times more likely to end up in the back of an ambulance than users of natural cannabis. Mike Power, Guardian, 10 May
expensive testing of the substances in specialised laboratories, and there is simply no budget big enough to carry out the work. A legal logjam awaits. Yet these drugs are not safe: users of synthetic cannabis are 30 times more likely to end up in the back of an ambulance than users of natural cannabis. Mike Power, Guardian, 10 May
 MAYORAL PRIORITIES
MAYORAL PRIORITIES





 UK governments agree that above all what they want out of treatment is ‘recovery’. Some of the most marginal, damaged and unconventional of people are to become variously abstinent from illegal drugs and/or free of dependence and (as Scotland’s strategy put it) ‘active and contributing member[s] of society’, an ambition which echoes those of the UK government dating back to the mid-2000s for more drug users to leave treatment, come off benefits, and get back to work.
UK governments agree that above all what they want out of treatment is ‘recovery’. Some of the most marginal, damaged and unconventional of people are to become variously abstinent from illegal drugs and/or free of dependence and (as Scotland’s strategy put it) ‘active and contributing member[s] of society’, an ambition which echoes those of the UK government dating back to the mid-2000s for more drug users to leave treatment, come off benefits, and get back to work.







 STREETS AHEAD
STREETS AHEAD discouraging their diversion for illicit purposes,’ says the Home Office. Documents at
discouraging their diversion for illicit purposes,’ says the Home Office. Documents at 

 Aspire’s New Beginnings Recovery-Orientated Detoxification Service joined organisations around the UK to raise awareness of depression while removing stigma surrounding the condition.
Aspire’s New Beginnings Recovery-Orientated Detoxification Service joined organisations around the UK to raise awareness of depression while removing stigma surrounding the condition.

Peer-led progress
It’s two years since the recovery documentary Dear Albert premiered at the International Film Festival in Calgary. A lot’s happened since then. Our peer-led programme ‘You do the MAFS’ (Mutual Aid Facilitation Services) has been further developed and is currently helping people in Leicestershire address substance misuse.
Today we have ambitions to help many more. The plan is to make our services available as an ‘off the shelf package’ so other communities benefit. Talk of devolving services to those that have been nearer the problem isn’t new. What’s new is that Dear Albert is realising what the sustainable model looks like.
It’s a model that provides recovery communities directly with earned income – services purchased by commissioners, main providers and others successfully delivered by recovery community members. So the mechanism is born to develop what I call the ‘purple pound’ by dispersing income to those in recovery. And for those that consider recovery communities a myth, let me tell you – I live in one.
But it’s mainly about partnerships. It’s about collaborative enterprise that works in unison with bigger providers and community assets to create longer-term solutions. Part of our start-up funding and support came through the University of Leicester’s Enterprise Inc2 project and the Leicester Recovery Partnership’s innovation fund. Now we’re delivering group work in HMP Leicester and also in the community via West Leicestershire clinical commissioning group. Our latest partnership is with Turning Point.
The exciting news is we’ve had a six-month evaluation of ‘You do the MAFs’ published in the Journal of Groups in Addiction and Recovery. The findings are very positive, highlighting the benefits of our structured and intensive pathway into mutual aid. Bridging this gap through better formal peer-led mechanisms like ‘You do the MAFs’ suggests more service users attending mutual aid and that they can continue to increase aspects of their recovery as a consequence.
The fact that we can use this intervention to support our own recovery communities is the icing on the cake. It’s great to see that the work we do here is starting to be recognised elsewhere and that we are able to contribute to the evidence base. We use interventions such as peer-led ACT and the Dear Albert film and have refined our messaging to create a whole package that gets the message across that people do recover, and helps identify the best route for each individual.
Securing the structure by which other communities can start generating their own income by using ‘You do the MAFs’ is Dear Albert’s next step. The basic model – Independent peer-led facilitation into existing community assets – is already in place.
Jon Roberts is director of Dear Albert, www.dearalbert.co.uk