A once-in-a-lifetime opportunity to finally eliminate hepatitis C is within our grasp, says Professor Ashley Brown.
Read the full article in October DDN Magazine

When I first graduated in medicine, hepatitis C didn’t even have a name, let alone a cure. The clinical condition characterised by low-level inflammation leading to liver fibrosis, and in some cases to cirrhosis, liver failure and liver cancer, was known as ‘non-A-non-B hepatitis’. Once the virus had finally been isolated and identified in the late 1980s, it acquired a catchier name, joining the alphabet of viral hepatitides as hepatitis C (HCV). In the 30 years since I began practising, the shift from this earlier era of ignorance to the current possibility for elimination has been unprecedented in the history of medicine.
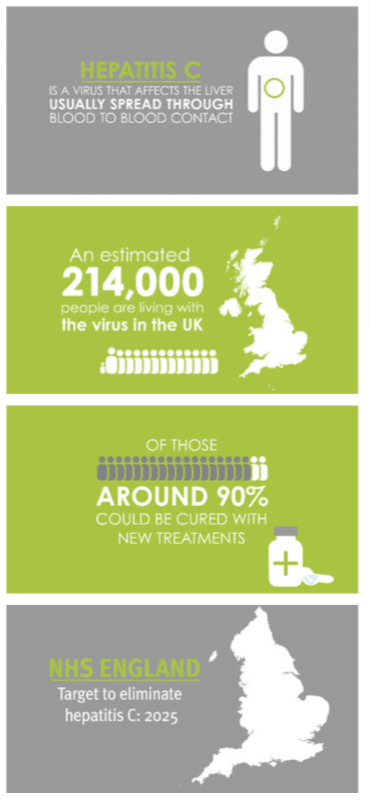
Hepatitis C is a blood-borne virus, meaning that it is transmitted through blood-to-blood contact, such as getting a tattoo with an unclean needle or receiving treatment in a country or environment where inadequately sterilised medical or dental equipment is reused. An estimated 4,000 haemophiliacs in the UK were infected with HCV when they received contaminated blood products prior to the initiation of screening blood donations in 1991. But the most common method of transmission in the UK today is through the sharing of needles and other drug paraphernalia.
 It has been estimated that around half of all people who inject drugs (PWIDs) have been exposed to the virus at some point. Because of the social stigma and legal issues surrounding drug use, hepatitis C brings with it a raft of shame, ignorance, and fear. Many people resist testing because they don’t want to be ‘in the system’, while others experience no symptoms so feel there is no hurry to test. Sadly a stigma exists that rivals HIV in the 1980s, which we need to dispel so that people are less fearful about finding out their HCV status.
It has been estimated that around half of all people who inject drugs (PWIDs) have been exposed to the virus at some point. Because of the social stigma and legal issues surrounding drug use, hepatitis C brings with it a raft of shame, ignorance, and fear. Many people resist testing because they don’t want to be ‘in the system’, while others experience no symptoms so feel there is no hurry to test. Sadly a stigma exists that rivals HIV in the 1980s, which we need to dispel so that people are less fearful about finding out their HCV status.
In the early years of attempting to treat this virus, clinicians believed that by boosting the immune system with very high doses of interferon – a substance produced naturally in response to viral infections – HCV infection could be overcome. This early treatment was successful in beating the virus in between 30 and 60 per cent of cases, but this limited success came at a high price. The flu-like side effects were deeply unpleasant and often intolerable, and the treatment could also trigger depression and exacerbate other mental health issues. Worse still, the drug had to be injected, a major deterrent for many recovering drug users. This meant that many people at risk refused even to test for HCV, let alone contemplate treatment.
Thankfully we have moved on from the dark days of interferon-based treatments to an era where cure is not just possible but highly probable. A pharmaceutical revolution has resulted in the development of a whole range of highly effective drugs called direct-acting antivirals (DAAs) that target the virus directly, with minimal side effects, and can cure it in more than 95 per cent of cases.
These incredible medicines provide us with an opportunity to eliminate HCV as a public health concern. The challenge has already been laid down by NHS England, which announced earlier this year that it was aiming to make England the first country in the world to eliminate hepatitis C by 2025 – a full five years ahead of the World Health Organization (WHO) global target.
However, two major obstacles remain in our way. Firstly, since the majority of people living with HCV are unaware of their infection we need to ensure that all those who may be at risk are given appropriate information and offered testing and pathways into treatment. Secondly, there are many who have been diagnosed but due to lifestyle, stigma or ignorance of advances in treatment have disengaged from treatment services.
To overcome the first obstacle we need to understand that hepatitis C is a disease of vulnerable people who might lead chaotic lifestyles, which means testing and treatment must be available where these groups access care – not only in hospitals and GP surgeries but homeless shelters, needle exchanges, sexual health clinics, pharmacies and amongst the prison population.
We know from peer-to-peer conversations that out-of-date misinformation about diagnosis and treatment persists, dissuading those who would benefit from treatment from coming forward to receive it. All healthcare professionals therefore need to make it clear that the days of the brutal interferon treatments are over, and that simple, short, well-tolerated oral drug combinations are available to all.
In order to overcome the second we need to radically reconfigure existing HCV treatment services. Commissioners need to be asking about HCV treatment delivery in their area, and we have to accept that many who need treatment will simply not conform to classical care pathways. New treatments are straightforward to take and can be delivered effectively in the community, and those who have adapted are already seeing the benefits in terms of increased treatment numbers and patient satisfaction.
Here in West London I am fortunate to work with a team people who are proactive and committed, and prepared to go beyond the normal call of duty. My specialist nurses already offer counselling, testing and treatment in a whole range of locations including drug and alcohol services, sexual health clinics, homeless hostels, needle/syringe exchanges and mental health facilities. One consultant colleague is offering clinics in a GP surgery that caters to marginalised communities and another is piloting a scheme for point-of-care testing in community pharmacies.
Along with my PhD fellow I have established an in-reach service at the local prison, HMP Wormwood Scrubs, and while it has taken some time to navigate the prison bureaucracy the service is already paying dividends with increasing numbers of prisoners accessing treatment. Additionally, I am working hard to reconnect with patients who have fallen out of contact with services.
While NHS England and Public Health England quite rightly focus on the statistics – already we have seen a significant decrease in the demand for liver transplant for HCV and hospital admissions due to HCV-related liver failure – what drives those of us who work on the ground is the individual human benefit that each and every patient derives from treatment. The physical and psychological benefit of clearing a virus that can potentially lead to cancer or premature death is immeasurable, as are the benefits to society of a healthier, happier workforce. The walls of our clinics are covered with ‘Thank You’ cards from grateful patients – one that brought a tear to my eye was from a young girl who simply said ‘Thank you for giving me my Grandpa back.’
The transformation of HCV from an unknown virus to potential global elimination within a single career lifetime is truly a one-off event, and the possibility for a genuine public health success story remains within our grasp. But this will only be achieved by education of public and professionals alike, and a willingness from all parties to adapt. With your help, I hope we can put this ‘silent killer’ to bed before I collect my pension.
