There are set principles that anyone working with people with complex needs should adhere to, say Dr Stephen Donaldson, Ben Sweeting, Richard Croall and Edward Loveless.
 Multiple disadvantage is a term used to describe people who have experienced or are experiencing multiple difficulties, including repeat street homelessness, trauma, substance misuse, physical health difficulties and mental health problems. These challenges often – and understandably – impact on people’s engagement with services, psychological wellbeing, physical safety, and sense of connection with society. People faced with these challenges regularly fall between the gaps of services and, over time, hope and trust in others can be lost. This can lead to people feeling trapped in a cycle of wanting help, not asking for help or asking in ways that communicate their distress through behaviours which are harder for some to understand.
Multiple disadvantage is a term used to describe people who have experienced or are experiencing multiple difficulties, including repeat street homelessness, trauma, substance misuse, physical health difficulties and mental health problems. These challenges often – and understandably – impact on people’s engagement with services, psychological wellbeing, physical safety, and sense of connection with society. People faced with these challenges regularly fall between the gaps of services and, over time, hope and trust in others can be lost. This can lead to people feeling trapped in a cycle of wanting help, not asking for help or asking in ways that communicate their distress through behaviours which are harder for some to understand.
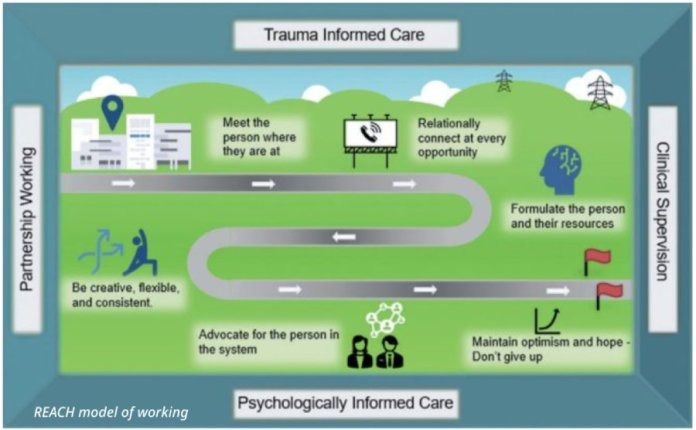
The REACH (Reducing Exclusion for Adults with Complex Housing Needs) team was set up to work with those who are street homeless and experiencing mental health difficulties and substance misuse in Scarborough and Whitby.
The team takes a partnership approach with multiple service partners coming together to support the person in their journey of recovery. Our vision is to support people to have housing stability, through a Housing First model. But while having a home is important, it’s only the tip of the iceberg. Given the multiple disadvantages experienced, working with people to help them manage addiction, trauma, and their mental health difficulties is key to stability and change. Everyone deserves to have a life worth living, but this can be a long and bumpy road to travel.
As part of our developing work in the area, we’ve been reflecting on some of the shared principles we hold to guide what we do, with the hope of developing practice-based evidence in this area.
PRINCIPLES OF WORKING
We developed a set of guiding principles to support the interventions and work we do.
- MEET THE PERSON WHERE THEY ARE AT
This principle, given the repeat homelessness experienced by this client group, is both physical – in terms of being present with people on the street – and psychological, in terms of acknowledging that traditional approaches to assessment, formulation, safety planning, care planning and intervention all need adapting to support the person. It’s also important to think about the reality of the person’s position and ensure that goals and expectations around engagement are realistic and don’t set people up to fail, preventing a further cycle of service disconnection, abandonment, and perceived failure.
- RELATIONAL CONNECTION AT EVERY OPPORTUNITY
As past trauma is a significant contributor to substance misuse and mental health issues, it’s essential that every contact takes a relational-trauma informed stance. Each contact has the potential to harm or heal, and therefore the primary focus is on building a psychologically safe frame within which therapeutic attachment and intervention can take place. This ensures that the people we work with can feel emotionally and psychologically safe.
- FORMULATE THE PERSON AND THEIR RESOURCES
Often people are referred to our service with a collection of labels, diagnoses and narratives, and what can get lost is the person’s story and experiences. Within our model, hearing the person’s narrative of their experiences and resourcefulness, alongside their challenges, is significant. Having a co-created, shared narrative helps the person feel heard, while also ensuring that an understanding of what has happened to them – and how we may be able to help – is realistic and transparent.
- BE CREATIVE, FLEXIBLE, AND CONSISTENT
To work with people who have experienced substance misuse, mental health, loss and trauma requires a great deal of creativity and flexibility. This can mean a significant adaptation of how we’ve traditionally gone about engaging with people. However, it’s equally important that there is consistency, boundaries and clarity in the approach. Often people have felt let down and abandoned, so consistency in engagement is paramount to rebuilding a sense of trust, while boundaries offer a sense of physical and psychological safety. This process is not without its challenges, with ruptures and repairs within the therapeutic relationship being a common and often necessary part of the trust building process. For clinicians, openness, curiosity and not enacting rejecting or rescuing behaviour is key.
- ADVOCATE FOR THE PERSON IN THE SYSTEM
Organisational systems and processes are complex and can, for many service users, feel difficult to negotiate. It’s therefore key that we advocate alongside the person to help them access what they need. However, it’s very common for people to be seen as hard to help as a result of stigma and harmful narratives. These narratives and experiences of rejection have often exacerbated a sense of disconnection from society and loss of hope for many of those we work with. Advocating for the person is important in supporting change, but there’s also a significant role in supporting the wider system to challenge its own views, narratives, and ideas about people and the ways they present.
- MAINTAIN OPTIMISM AND HOPE – DON’T GIVE UP
Given the multifaceted nature of the difficulties and challenges the people we work with face and present with, it can feel clinically overwhelming at times. A cyclical process of change-stability-lapse-relapse-change is the norm. For many professionals this process can challenge the fundamental values of why we work in this field, our own sense of clinical competence and at times lead to a perception of not being good enough at our jobs. For this client group this can be experienced as rejection – where they’re seen as too complex and passed to someone else or told they need something else, further exacerbating a sense of hopelessness. Having access to regular, consistent and skilled psychological supervision is therefore a must-have.
This approach of a psychologically informed frame is not easy, and can face constant challenges. However, it’s ultimately the only way to consistently support stability and recovery for those with complex homelessness, substance misuse and mental health needs. By ensuring this frame and its principles are in place and constantly reflected on maintains clinical optimism, shared understanding, and collaborative partnership working. Overall, this approach ensures that the care provided is stabilising rather than inadvertently damaging, thus working to reduce further trauma and enhance the quality of life of those in need.

Dr Stephen Donaldson is consultant clinical psychologist, Ben Sweeting is advance nurse practitioner, mental health, and Richard Croall is advance nurse practitioner, dual diagnosis – all at the REACH team. Edward Loveless is assistant psychologist, Tees, Esk and Wear Valley’s NHS Foundation Trust.
